 Lasix Side Effects: What You Need to Know
Lasix Side Effects: What You Need to Know
Lasix, known generically as furosemide, is a powerful loop diuretic utilized primarily to reduce edema (swelling) and manage high blood pressure, conditions often seen in patients with heart failure, liver disease, and kidney dysfunction. By preventing the absorption of sodium and chloride in the kidney tubules, it promotes the expulsion of these ions and water from the body. While its effectiveness in removing excess fluid from the body is life-saving, it comes with a spectrum of potential risks and side effects that cannot be overlooked. The rapid fluid loss can lead to dehydration, electrolyte imbalances, and alterations in blood volume, potentially exacerbating the very conditions it is meant to mitigate.
Understanding the inherent risks associated with Lasix is crucial for both healthcare professionals and patients. Dehydration and electrolyte imbalances, for instance, can manifest as muscle cramps, weakness, dizziness, confusion, and increased heart rate. Prolonged use or high doses can also place additional strain on the kidneys, potentially leading to or worsening renal impairment. It is, therefore, imperative to monitor patients closely, adjusting dosages as necessary to strike a delicate balance between therapeutic effectiveness and minimizing adverse effects. Awareness and early detection of side effects can make a significant difference in patient outcomes, emphasizing the importance of informed use of Lasix in clinical practice.
Thirsty No More? Think Again: Lasix and Dehydration
Lasix, a diuretic commonly prescribed for managing fluid retention and hypertension, works by increasing the amount of urine produced, thereby assisting the body in eliminating excess fluid. However, this mechanism of action can lead to significant dehydration if not carefully monitored. Dehydration from Lasix is not just a minor inconvenience; it can be severe, affecting various bodily functions and leading to symptoms such as dizziness, dry mouth, thirst, weakness, lethargy, and confusion. The risk of dehydration underscores the importance of patients being vigilant about their fluid intake and healthcare providers closely monitoring their patients' hydration status.
The dehydration risk associated with Lasix necessitates a cautious balance of fluid management. Patients taking Lasix should be educated about the signs of dehydration and the importance of maintaining adequate fluid intake. It is crucial for patients to communicate any symptoms of dehydration to their healthcare provider promptly. Additionally, healthcare providers may need to adjust the dosage or frequency of Lasix administration to mitigate dehydration risks, highlighting the need for tailored treatment plans and regular follow-up appointments to monitor the patient's response to the medication and their hydration levels.
Listening to Your Body: Recognizing Lasix-induced Hearing Loss
One of the lesser-known but significant side effects of Lasix, a widely used diuretic, involves its potential to affect hearing. While Lasix is effective in removing excess fluid from the body, it can also cause rapid changes in the composition of body fluids, leading to ototoxicity - a toxic effect on the ear structures. This condition may manifest as ringing in the ears (tinnitus), hearing loss, or even temporary deafness, especially when the medication is administered in high doses or intravenously. Patients are advised to monitor any changes in their hearing and consult their healthcare provider immediately should any abnormalities occur.
Understanding and being vigilant about the auditory implications of taking Lasix is critical for individuals relying on this medication. The risk of hearing loss is particularly pronounced in patients with renal impairment or those on concurrent medication that has ototoxic potential. Proactive measures, including regular hearing tests and discussing medication adjustments with healthcare providers, can help mitigate the risk. It’s crucial for patients to report any hearing discrepancies as early as possible to avoid long-term damage, emphasizing the importance of listening to and understanding the signals their bodies may be sending.
The Balancing Act: Lasix's Impact on Kidney Function
Lasix, a powerful diuretic, plays a significant role in managing fluid retention and swelling in conditions involving the heart, liver, or kidneys. However, its mechanism of increasing urine production to expel excess water and salt from the body demands careful monitoring of kidney function. Overuse or prolonged administration can strain the kidneys, potentially leading to alterations in kidney performance. This delicate balance necessitates regular kidney function tests to ensure that Lasix's diuretic benefits do not tip into detrimental effects, underlining the importance of healthcare provider oversight in managing dosage and duration of treatment.
Patients on Lasix may experience changes in kidney function markers, such as increased creatinine or reduced glomerular filtration rate, signs that the kidneys are under pressure from the medication's diuretic effect. These changes could signal the need for adjustment in therapy or additional measures to support kidney health. Awareness and proactive monitoring are key to preventing potential kidney-related complications. By maintaining an open dialogue with healthcare practitioners and reporting any unusual symptoms promptly, patients can help safeguard their kidney health while benefiting from Lasix's therapeutic effects.
When Vision Gets Blurry: Understanding Lasix's Ocular Side Effects
Lasix, commonly known for its prowess in treating fluid retention related to heart failure, liver disease, and kidney disease, also possesses a lesser-known side effect that can impact one's vision. The drug can lead to temporary or, in rare cases, permanent visual disturbances. Patients may experience blurred vision, a decrease in visual acuity, and in some instances, a condition known as acute transient myopia. This sudden shift in vision can be disconcerting, prompting an immediate need for medical consultation to adjust the medication or explore alternative treatments.
The mechanism behind these ocular side effects remains a subject of research, but it is believed that Lasix can alter the pressure within the eye, potentially leading to complications such as glaucoma in susceptible individuals. Furthermore, the rapid alteration in body fluid levels caused by Lasix may affect the lens and other parts of the eye, leading to changes in vision. It is crucial for patients on Lasix to monitor any visual changes closely and report them to their healthcare provider for a thorough examination and appropriate management to prevent long-term implications on their eyesight.
From Rays to Rashes: Lasix and Increased Sun Sensitivity
Lasix, while widely prescribed for its efficacy in treating fluid retention and related conditions, carries a lesser-known risk tied to sun exposure. Individuals taking this medication may find themselves more sensitive to sunlight, a condition medically referred to as photosensitivity. This heightened vulnerability necessitates a cautious approach to sun exposure, as the skin can react more severely to ultraviolet (UV) rays, leading to sunburns that are more intense than usual. The phenomenon is attributed to Lasix's interaction with skin cells, altering their natural protective response against UV radiation.
Adopting protective measures becomes paramount for patients on Lasix, underscoring the importance of comprehensive sun protection strategies. This includes the application of high SPF sunscreens, wearing protective clothing, and seeking shade during peak sunlight hours. Awareness and proactive management of this side effect can significantly mitigate the risks of photosensitive reactions. Patients are also encouraged to consult their healthcare provider for personalized advice and to discuss any concerning symptoms, such as rash or severe sunburn, that may arise from sun exposure while on Lasix.
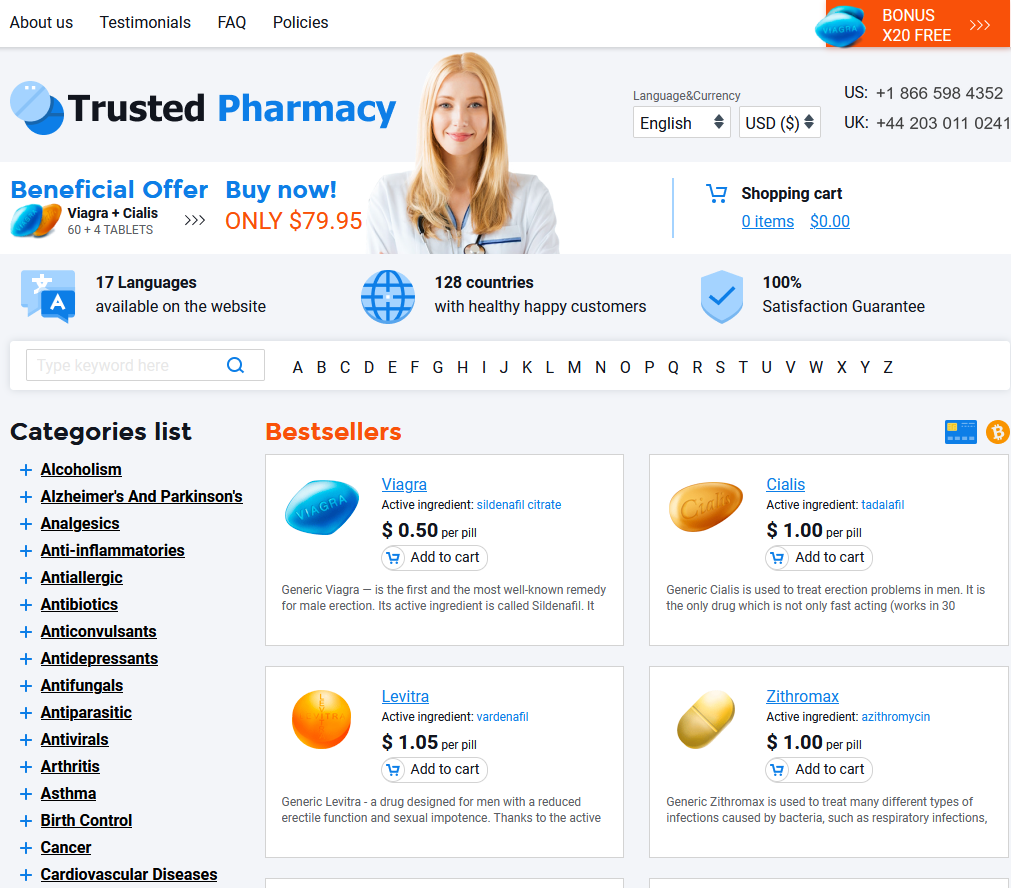
clomiphene for sale purchase lasix buy Bactroban online
